All anxiety disorders fit under the umbrella of ‘anxiety’ as all the disorders have elements of fear, anxiety, and or worry associated with the experience of the person.
With every disorder, both mental health disorder and physical health disorder is seen and felt differently. What we are talking about here are the common elements and the diagnostic criteria for each disorder.
While there is a kind of ‘box’ of what is needed to meet a diagnosis, how you see a disorder and live it in your life maybe slightly or completely different to someone else.
There also needs to be a spectrum here as while you may meet the diagnoses criteria some people experience the extremes of certain symptoms that are unbearable in comparison to others who can remain able to continue living their lives in the way they want to.
Let’s look at the following Anxiety Disorders:
- Generalised Anxiety Disorder (GAD)
- Obsessive Compulsive Disorder (OCD)
- Social Phobia
A caution: The ‘diagnoses box’
The diagnosis box needs to be raised as for some people a diagnosis and being placed in certain criteria can be positive and for others, it can be negative. For some it’s a relief that what they are going through has a ‘name for it’ and therefore they can talk about it more easily, identify triggers and what works and start working on it.
For others, the diagnosis box is too small, confined and feels too clinical and labelling. Historically some patients were named after their diagnoses, like there goes OCD, de-identifying the person and completely disregarding them as human first. In our work, we often use the word ‘experience’ because how you deal with, work through and label things maybe completely different to someone else. That is OK.
Generalised Anxiety Disorder, AKA GAD
The following are needed to match the criteria for GAD:
- Excessive anxiety or worry , occurring more days than not for 6 months or more about different events or activities.
- The individual finds it difficult to control the worry.
- The anxiety and worry are associated with 3 or more of the following: 1 restlessness or feeling keyed up 2 Being easily fatigued 3 Difficult concentrating or mind going blank 4 Irritability 5 muscle tension 6 sleep disturbance.
- The anxiety or worry or physical symptoms affect the person’s functioning in daily life.
- The disturbance is not because of alcohol or other drugs.
- The disturbance is not better explained by another disorder.
The key point of difference is that GAD is long standing and the worry experienced is focused on more than 1 event or issue. People with GAD can sometimes forget when they were last in a relaxed state. The physical and mental symptoms are varied from person to person and can be mild or extreme.
Obsessive Compulsive Disorder, AKA OCD
The following are needed to meet the criteria for OCD:
Part A
The presence of obsessions, compulsions, or both
Obsessions are defined as:
- Recurrent and persistence thoughts that are unwanted which cause anxiety and or distress and
- The individual tries to suppress or ignore such thoughts, urges or images or tires to neutralise them by completing a compulsion behaviour
Compulsions are defined by
- Repetitive behaviours (eg hand washing) or mental acts (praying) that the individual feels driven to perform in response to an obsession and
- The behaviours or acts are performed in order to reduce anxiety or distress.
In reality these behaviours have no rational connection with preventing the anxiety or dreaded event (eg hand washing to prevent being hit by a car)
Part B
The obsessions or compulsions are time consuming or cause significant distress which impacts the persons functioning in daily life
Part C
The obsessions/compulsions are not attributed to the effects of a substance
Part D
The Obsessions and compulsions cannot be attributed to another mental disorder (eg excessive worry attributed to Generalised Anxiety Disorder).
Part D needs to explored thoroughly as there are many different attributes that obsessions and compulsions can come from. Another element is hat the person recognises that the obsessions and compulsions are excessive and unreasonable in nature. Poor insight reflects difficulty in being treated for the disorder.
OCD is the fourth most common mental illness after major depression, substance abuse and phobias.People with OCD have repetitive thoughts or images that they can’t control, and the anxiety caused by these thoughts leads to impulses or actions that are distressing, time-consuming or limiting to normal functioning.
Although a person’s symptoms may change over time, it appears that they often stay within the same symptom group for a given individual.
There are four groups commonly described, that include:
- Contamination and cleaning symptoms,
- Hoarding obsessions and compulsions,
- Symmetry/ordering/repeating symptoms and
- Aggressive/religious/sexual/somatic and checking symptoms.
Social Phobia
The following are needed to meet the criteria for Social Phobia, AKA Social Anxiety Disorder
- A persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others. The individual fears that they will act in a way (or show anxiety symptoms) that will be embarrassing and humiliating.
- Exposure to the feared situation almost invariably provokes anxiety, which may take the form of a situationally bound or situationally pre-disposed Panic Attack.
- The person recognizes that this fear is unreasonable or excessive.
- The feared situations are avoided or else are endured with intense anxiety and distress.
- The avoidance, anxious anticipation, or distress in the feared social or performance situation(s) interferes significantly with the person’s normal routine, occupational (academic) functioning, or social activities or relationships, or there is marked distress about having the phobia.
- The fear, anxiety, or avoidance is persistent, typically lasting 6 or more months.
- The fear or avoidance is not due to direct physiological effects of a substance (e.g. drugs, medications) or a general medical condition not better accounted for by another mental disorder.
Some common trouble areas for people with Social Phobia are, dating, making eye contact, speaking to strangers, going to parties, using public restrooms, and/or eating in front of others.
These trouble areas are focused on by the person and the time spent worrying impacts the person’s normal level of functioning. This disorder can be extremely isolating for people and be misinterpreted by some as just being ‘shy’.
The person with social phobia may also have underlying fears related to looking foolish, worrying about other people noticing their physical symptoms, looking quiet or boring to others and/or being judges as being socially inadequate.
Recovery
Recovery from any mental illness is possible. For some, recovery might be improved functioning so you’re able to return to work or get out of the house. Or it might be total recovery from the mental illness from all parts of your life.
Yes, mental illness can come up again in your life in a stressful period, particularly anxiety disorders but the grip on your life can reduce with the right support. So in your life what does one step closer to recovery look like? It’s best to think of a small step like building a toolkit of strategies and trying them out.
By having a few tools can be a great way to feel more in control in knowing you can try something that can work and has worked for others.
Understanding your mental illness is really important but also to share your experience with others. This can be scary but in doing this you are opening up what is going on for you and rallying support.
All of these disorders need professional mental health help from a practitioner who can be in your corner, understand your experience and work with you towards recovery.
There are reasons why anxiety is taking up space in your life and we want to unpack this with you in a safe environment.
We want to hear from you!
Our mental health professionals are ready and willing to hear from you and hear your story of mental health. Do you have some questions or want to know more about what may help?
We provide a number of counselling options for you in Melbourne – in Footscray – as well as online, Australia-wide.
Take the time and reach out today.
Some basic tools for your anxiety disorder
Grounding
What happens with anxiety is that all of our energy is taken up by our brain, consumed by disturbing thoughts. These thoughts go around and around and we don’t feel like we are present in our bodies. Grounding helps by moving away from our thoughts to feeling more present.
- Sit yourself on a sturdy chair with your bum on the edge of the sit.
- Put your feet firmly on the ground (shoes on or off is fine)
- Now this is going to sound weird but start to wiggle your toes. Notice how weird it feels, notice your toes in your shoes or freely moving on the ground.
- Next, push your feet on the ground pushing your knees with your hands. Push hard downwards for 30 secs.
- Now relax and stop pushing, notice what it feels like, notice the relaxed state of your feet.
- Try again, pushing into the ground and now at the same time wiggle your toes. Push and wiggle.
- And relax again. Notice being relaxed. You can do this a number of times if you need to. But have a break if you feel it isn’t changing your anxiety level.
Anxiety Scale
Anxiety usually comes in waves with a panic attack being a 10 out of 10. And 0 being no anxiety and very happy and engaged in your day. Everyone’s anxiety scale is different and unique as your presentation of a 10 may look different to somebody else’s 10.
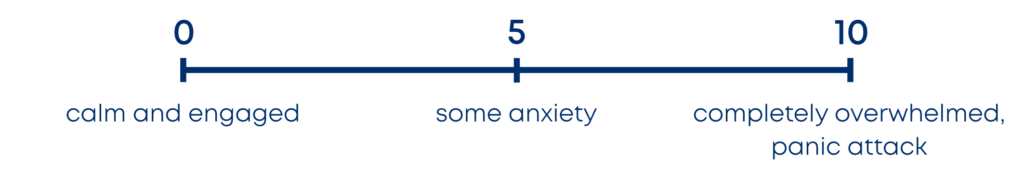
So for some people 0 is off the table. It can seem kind of foreign as it has been a long time since they have felt calm.
That’s OK for now. It’s just about understanding where you are at and then figuring what helps you at that number.
At 10, many people can’t talk and trying to have a conversation makes things worse. But maybe being in a dark room hugging a pillow with soft music may help.
At 5 it might be helpful to talk to a friend or start to write about your anxiety. For everyone their experience of anxiety is individual but some tools can help.
The anxiety scale is a good resource to use to help you be mindful of your number. Then you can put in place an action plan.
Here are some quick videos to help slow down anxiety